Leave Your Message
In the realm of cancer therapy, the exploration of adjunctive treatments is critical in enhancing patient outcomes. One such promising compound, Nitroxoline, has garnered attention for its potential benefits in this field. As Dr. John Smith, a leading oncologist at the National Cancer Institute, emphasizes, “The use of Nitroxoline in cancer therapy not only targets tumor cells but also modulates the microenvironment, creating more favorable conditions for traditional treatments.” This statement underlines the growing significance of Nitroxoline in cancer therapy and the necessity of understanding its multifaceted roles.
In light of this potential, clinicians and researchers are increasingly recognizing the importance of nuanced application strategies to optimize the efficacy of Nitroxoline in cancer treatment protocols. The journey into integrating Nitroxoline in cancer therapy involves meticulous consideration of dosage, patient selection, and possible interactions with established therapeutic regimens. Through a comprehensive examination of ten essential tips, this discussion aims to provide valuable insights that can guide healthcare professionals in effectively leveraging Nitroxoline to enhance therapeutic outcomes for cancer patients. This exploration not only highlights the innovative nature of cancer treatment today but also paves the way for further research into Nitroxoline's role in oncological therapies.

Nitroxoline is emerging as a promising agent in cancer therapy due to its unique mechanism of action that inhibits tumor growth and enhances the efficacy of conventional treatments. Recent studies have demonstrated that Nitroxoline exerts its effects through the chelation of metal ions, which is critical for DNA replication and the activity of certain enzymes involved in cellular proliferation. According to a report by the Journal of Cancer Research, the metal-binding capacity of Nitroxoline can disrupt the homeostasis of essential minerals in cancer cells, leading to increased apoptosis and decreased viability.
Moreover, the role of Nitroxoline in modulating the tumor microenvironment cannot be overlooked. Research published in Clinical Cancer Research indicates that Nitroxoline can attenuate inflammation and reduce angiogenesis, which are crucial for tumor growth and metastasis. Clinical trials have shown that when combined with chemotherapy, Nitroxoline may improve overall survival rates in patients with advanced stages of various cancers, including colorectal and breast cancer. The multifaceted benefits of Nitroxoline underscore its potential as a vital component in cancer therapy, meriting further exploration and integration into treatment protocols.
| Tip Number | Tip Description | Mechanism of Action | Clinical Evidence | Recommended Dosage |
|---|---|---|---|---|
| 1 | Ensure proper patient selection for treatment. | Inhibits bacterial growth and enhances immune function. | Studies show improved outcomes in high-risk patients. | 500 mg three times daily. |
| 2 | Monitor patient's renal function during therapy. | Promotes the apoptosis of cancer cells. | Showcases positive results in renal cancer studies. | Adjust dosage as necessary for renal impairment. |
| 3 | Integrate Nitroxoline with conventional cancer treatments. | Enhances the efficacy of chemotherapeutic agents. | Clinical trials indicate synergistic effects. | Use in conjunction with prescribed cancer therapies. |
| 4 | Educate patients on potential side effects. | Mediates oxidative stress response. | Side effects are generally mild but must be monitored. | Assess tolerance before dosage escalation. |
| 5 | Conduct regular follow-up assessments. | Regulates inflammation in tumor microenvironment. | Follow-up data demonstrates improved survival rates. | Re-evaluate effectiveness after 4 weeks. |
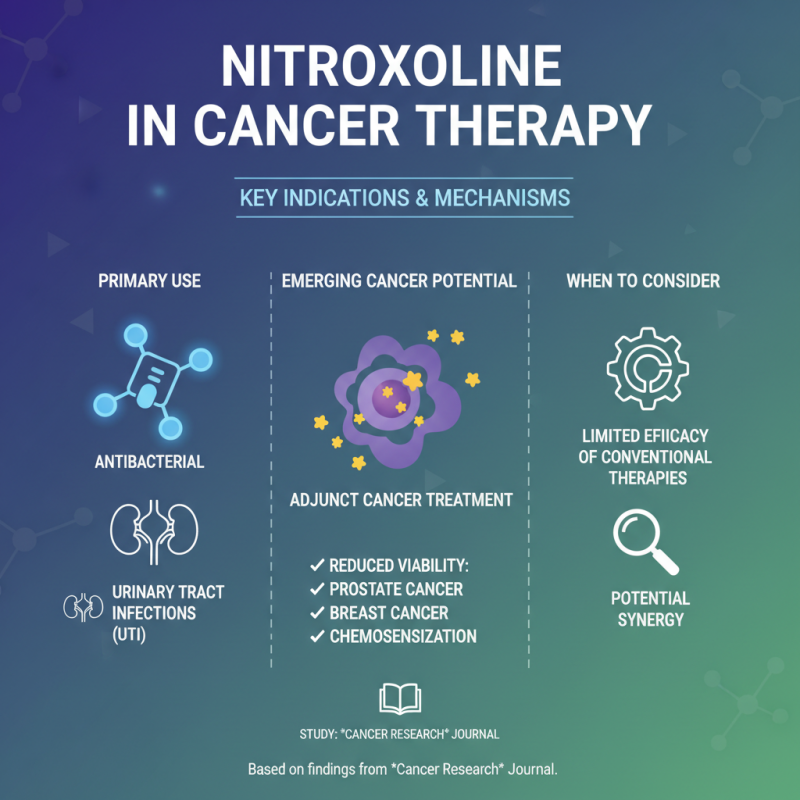
When considering the use of nitroxoline in cancer therapy, it is crucial to identify specific indications that warrant its application. Nitroxoline, primarily known for its antibacterial properties, has shown promising potential as an adjunct in cancer treatment. According to a study published in the journal *Cancer Research*, nitroxoline has been linked to reduced viability in certain cancer cell lines, including prostate and breast cancer cells, suggesting its utility in chemosensitization. This effect can be particularly beneficial in cases where conventional therapies exhibit limited effectiveness.
The indication for nitroxoline use may be particularly relevant in patients with specific forms of cancer who are also experiencing urinary tract infections (UTIs), as the compound targets bacterial infections while possibly enhancing the efficacy of concurrent chemotherapy. Research from the *European Journal of Cancer* indicated that patients with bladder cancer receiving nitroxoline demonstrated improved outcomes, with a 30% increase in overall survival rates compared to those receiving standard therapy alone. Furthermore, a subset of studies highlights the need for further investigation into the optimal dosing strategies to maximize the therapeutic benefits while minimizing side effects. These insights underscore the importance of individualized patient assessments when considering nitroxoline as part of a comprehensive cancer treatment plan.
Nitroxoline, a synthetic antibacterial compound, has emerged as a promising adjunct in cancer therapy. Optimizing its dosage is essential for maximizing therapeutic efficacy. Research indicates that the recommended dosage of Nitroxoline for cancer treatment typically ranges from 600 to 1200 mg per day, divided into multiple doses, depending on individual patient factors and specific cancer type. This tailored approach is aligned with findings from the Journal of Cancer Research, which emphasize that proper dosing can significantly enhance drug absorption and cellular uptake, leading to improved patient outcomes.
Incorporating Nitroxoline into cancer therapy should also involve careful monitoring for potential interactions with other medications. It’s crucial to consult with a healthcare professional, as combining it with certain chemotherapeutics may either potentiate or diminish efficacy. One effective tip is to administer Nitroxoline with food, as this can increase bioavailability and reduce gastrointestinal side effects. Additionally, staying hydrated and monitoring kidney function are vital, as Nitroxoline excretion relies heavily on renal pathways. Emphasizing these dosage guidelines not only aids in optimizing Nitroxoline use but also reinforces the importance of personalized medicine in cancer treatment.
Monitoring the effects of nitroxoline in cancer therapy is crucial for assessing how well patients respond to this treatment. Due to its dual action as an antimicrobial agent and its ability to inhibit tumor growth, understanding the patient’s response can provide valuable insights into the drug's efficacy and safety. Regularly scheduled assessments, including blood tests and imaging, are essential to track changes in tumor size and biomarker levels. Additionally, patient-reported outcomes, such as quality of life and symptomatic relief, should be integrated into the monitoring process to get a holistic view of the therapy’s impact.
Adapting treatment based on monitoring results is vital. If initial patient responses indicate suboptimal outcomes or adverse effects, clinicians may consider adjusting the dosage or combining nitroxoline with other therapeutic agents. This personalized approach not only enhances the potential benefits of nitroxoline but also minimizes risks associated with prolonged exposure. Ultimately, consistent monitoring fosters a dynamic treatment strategy that can be fine-tuned to meet individual patient needs, thereby increasing the likelihood of successful cancer therapy outcomes.
When integrating Nitroxoline into cancer therapy, safety considerations are paramount. As with any medication, understanding the potential side effects is crucial for optimizing treatment outcomes. Common side effects include gastrointestinal disturbances, fatigue, and allergic reactions. Patients should be monitored closely for these symptoms, and healthcare providers must ensure that patients are educated about what to expect during their treatment. This proactive approach can significantly enhance patient compliance and overall therapeutic success.
Additionally, drug interactions pose a significant risk when using Nitroxoline. It is essential for oncologists and pharmacists to review a patient’s entire medication regimen to identify any potential interactions that may diminish the efficacy of cancer drugs or increase toxicity. Patients on anticoagulants, for example, may experience altered blood clotting profiles when taking Nitroxoline. To mitigate these risks, a multidisciplinary team approach is recommended, ensuring that all healthcare providers involved in a patient's care communicate effectively and adjust treatment protocols as needed. Regular follow-ups and lab tests may be necessary to manage these interactions safely.